First, what is atrial fibrillation?
Atrial fibrillation (AF) is a common abnormal heart rhythm that happens when electrical impulses are triggered by different places in the atria (the upper chambers of the heart) in a disorganised way. This causes the atria to twitch and is felt as an irregular heartbeat or pulse.
The normal contraction of the muscle fibres of the atria typically allows for the coordinated and complete emptying of blood from the heart’s upper chambers into its lower ones (the ventricles).
Blood that is not completely pumped out of the atria can remain and may pool there (eventually resulting in blood clots). To maximise the efficiency of the heart and to avoid various diseases, the upper and lower chambers of the heart need to work in sync. That doesn’t happen during AF.
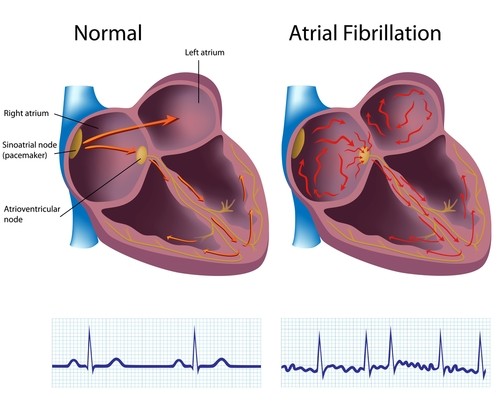
In AF, disordered or rapid electrical signals cause the atria to contract too quickly and chaotically (fibrillate). This leads to an irregular heartbeat referred to as ‘arrhythmia’.
AF is a serious condition that can occur without any signs or symptoms but can result in life-threatening complications if left untreated. Heart-related complications include blood clots, stroke (when the clot travels to the brain), and heart failure.
Atrial Fibrillation is a serious condition that can occur without any signs or symptoms but can result in life-threatening complications if left untreated.
By the numbers
The CDC (Centers for Disease Control and Prevention) reports that in the United States alone, 750,000 hospitalisations occur annually because of AF, which contributes to nearly 130,000 deaths each year.
AF costs the US about $6 billion every year. Medical costs for people who have AF are about 8-9 thousand dollars higher per year than for people who do not have AF.
Risks factors and symptoms
The most common cause of AF is abnormalities or damage to the heart’s structure. Patients are more likely to develop AF if they have high blood pressure, obesity, heart disease, diabetes, lung or kidney disease, or sleep apnoea. Those who have a family history of AF are also at risk.
Those who suffer from AF will most likely notice an irregular pulse. However, some people may only have mild symptoms, while others may exhibit no symptoms at all. These symptoms include palpitation (being aware of heartbeat), tiredness or fatigue, confusion, dizziness, shortness of breath, and chest discomfort (pressure) or pain.
Prevalence of Atrial Fibrillation
AF is the most common diagnosed arrhythmia in patients.
According to a 2013 study, AF is the most common arrhythmia worldwide and the estimated global age adjusted prevalence was 0.5% in 2010, representing nearly 33.5 million individuals. This is likely underestimated as a large number of people who do not exhibit symptoms but do have AF remain undiagnosed.
In the US, the CDC states that approximately 2% of people younger than 65 years old have AF and 9% of those older than 65 years.
What are the treatments for atrial fibrillation?
AF is mostly treated with lifestyle changes, medicines, procedures, and surgery to help prevent blood clots, slow the heartbeat, or restore the heart’s normal rhythm. Doctors will also look for any disease that may be causing it and assess the individual’s risk of developing dangerous blood clots.
Some people with AF need medications to help control the rate and rhythm of their heart. These medications are most commonly beta-blockers and anti-arrhythmic drugs.
Occasionally, a procedure such as ablation or cardioversion may be needed.
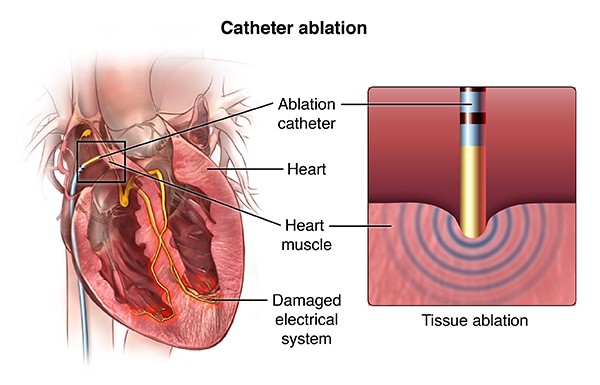
Cardiac ablation
If an AF patient is not responding well to medication, doctors would usually recommend cardiac (or catheter) ablation. It is a procedure that can correct heart rhythm problems (arrhythmias).
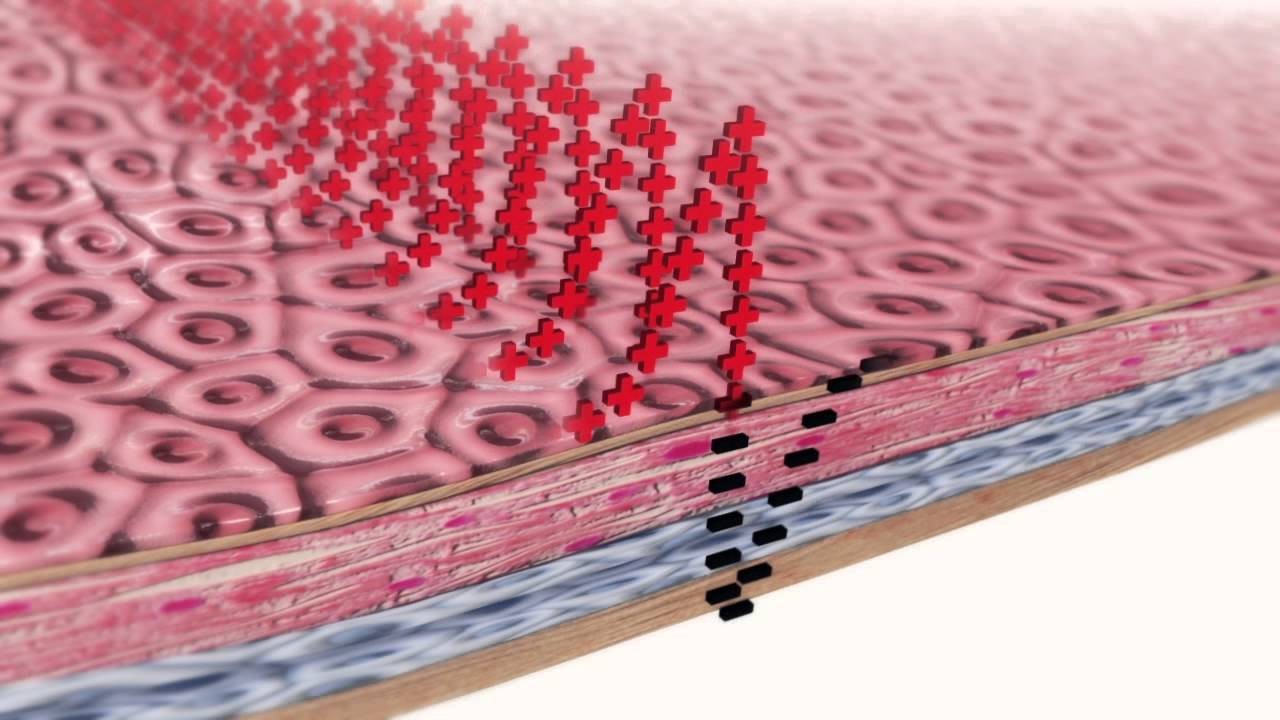
Cardiac ablation works by scarring or destroying tissue in the heart that triggers or sustains an abnormal heart rhythm. In some cases, cardiac ablation prevents abnormal electrical signals from entering the heart and, thus, stops the arrhythmia.
While cardiac ablation is sometimes done through open-heart surgery, it’s more often carried out using catheters that are less invasive, enabling shorter recovery times.
Cardiac ablation usually involves long, flexible tubes (catheters) inserted through a vein or artery in your groin and threaded to your heart, delivering energy in the form of heat or extreme cold to modify the tissues in your heart that cause an arrhythmia.
The Challenge with Persistent AF
AF is the most common clinically diagnosed arrhythmia with considerable impacts on public health. In some cases, patients suffer the ‘persistent’ type; arrhythmias that last from weeks to years.
For symptomatic patients who fail anti-arrhythmic drugs, pulmonary vein isolation (PVI) is the interventional approach of choice, particularly for patients with persistent AF.
However, the clinical outcomes of PVI for persistent AF have been disappointing, even with targeted ablation in place.
Accordingly, the appropriate ablation strategies for persistent AF remain the subject of intense debate. But what is clear is that the improvement in cardiac ablation outcomes will greatly depend on the precise identification and eradication of the functional drivers of AF located at sites distant to the pulmonary veins.
A key characteristic of patients with persistent AF is ‘continuous chaotic activation’, which means that potential ablation contact points along the atrial tissue need to be serially mapped over time. This renders the conventional 3D mapping that is based on voltage less effective.
Using advanced ultrasound for better imaging and mapping
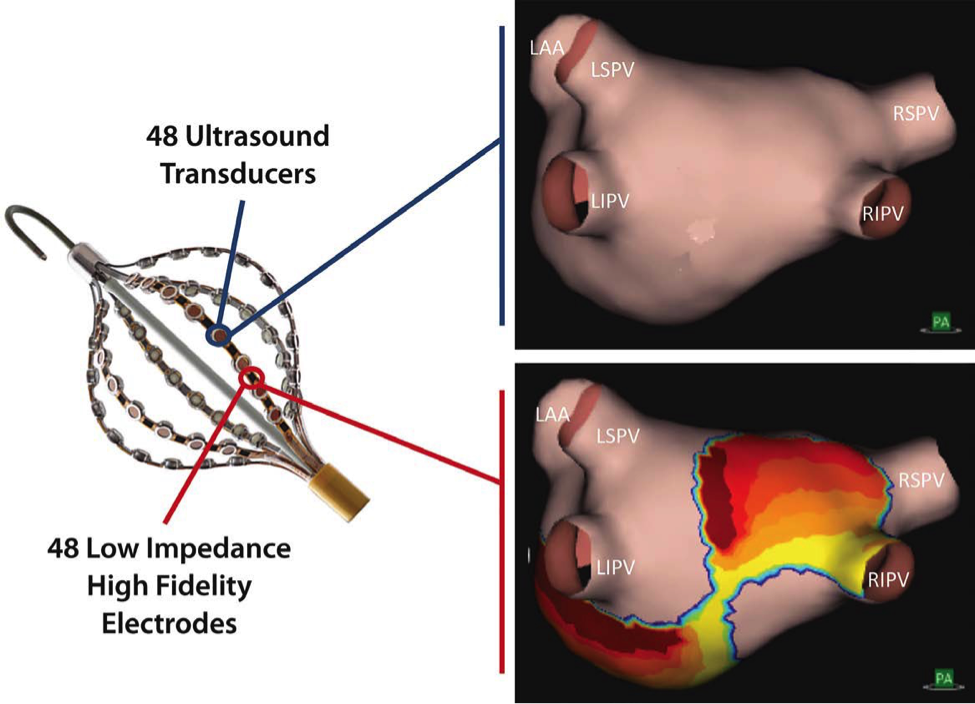
Acutus Medical®, Inc. has developed a novel, full-chamber, non-contact imaging, and mapping system that uses ultrasound to re-construct the patient’s heart anatomy and an algorithm to map its ‘charge density’ (CD). These ‘CD maps’ show the various electrical activation points that cause arrhythmia.
This new imaging and mapping system can output animated CD maps that are 4 times higher in resolution when compared to conventional voltage maps. It will effectively guide the doctor for the next cardiac ablation therapy.
As a result, ablation strategies can be individualised per patient to address dynamic activation patterns identified in addition to PVI.
The chamber surface is sampled from 48 ultrasound transducers distributed across 6 splines of the AcQMap catheter at an astounding rate of up to 115,000 surface points per minute. An anatomic image representing end-diastolic volume and shape is obtained from the points in less than 5 minutes and with a limited rotation of the catheter.
Clinical trials
Acutus performed a trial (dubbed ‘UNCOVER AF’) on 127 patients where they used the AcQMap system in combination with a variety of current ablation techniques.
Results from the trial indicated that 90% of patients had no recorded episodes of AF and 98% had <30% arrhythmia burden. The reduced levels of arrhythmia burden after CA were significantly associated with a clinically meaningful improvement in overall health status and quality of life.
Xeraya Capital and Acutus Medical®
Xeraya Capital is a proud partner and investor in Acutus Medical®. We firmly believe that better imaging, mapping, and diagnosis allows for increased effectiveness in treatments as doctors and physicians would know exactly where to look and act upon.
Initial tests with AcQMap have shown unprecedented clarity, and could greatly help physicians improve cardiac ablation outcomes by providing tailored therapy options and reducing the need for repeat procedures. Such an improvement can save time and procedure costs and, most importantly, makes life better for patients.
Sources:
- Targeting Nonpulmonary Vein Sources in Persistent Atrial Fibrillation Identified by Noncontact Charge Density Mapping (UNCOVER AF Trial) by Willems, et. al., CIRCEP.
- https://www.mayoclinic.org/tests-procedures/cardiac-ablation/about/pac-20384993
- https://heart.bmj.com/content/104/24/1989
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5460066/
- https://www.pharmacytimes.com/publications/health-system-edition/2016/january2016/novel-oral-anticoagulants
- https://www.healthline.com/health/living-with-atrial-fibrillation/facts-statistics-infographic#1