There are an estimated 7.6 billion people in the world right now, and as at March 2018, the World Health Organization (WHO) reports that 1.1 billion among us are smokers. The addiction to tobacco is simply one of the biggest public health threats the modern world has ever faced. Tobacco use kills up to half its users, and more than 7 million people die each year due to smoking. 6 million of those deaths are from direct tobacco use, and around 890 thousand more deaths are caused by non-smokers being exposed to second-hand smoke.
The socio-economic impacts of tobacco use are even more disturbing.
The Socio-Economic Impacts of Tobacco Use
According to the report by Action on Smoking & Health (ASH), the tobacco industry revenue was clocked in at $744 billion in 2014 alone. That’s more than the GDP of all but 18 nations combined. To put things in perspective, if tobacco corporations were a country, they’d be the 19th wealthiest nation.
How does this impact the rest of the world? Well, tobacco use burdens the global economy an estimated $1.4 trillion per year in healthcare and treatment costs related to tobacco-attributable diseases, as well as the cost of productivity loss due to smoking. Here’s something else to think about: 80% of the world’s 1.1 billion smokers live in low- to middle-income economies.
Smoking Cessation

Tobacco use (or simply ‘smoking’) is often regarded as a bad habit or a ‘vice’ so to speak. Smokers regard the addiction to tobacco use as something trivial until they want to quit. And the chances of successfully quitting are very small. Among smokers who are aware of the dangers of tobacco use, most want to quit. In the United States alone, more than 20 million smokers try to quit each year, with an average of 8-10 attempts per person.
Which is why most treatment plans encourage the act of ‘cessation’, as quitting is too ambitious and would often lead to various side-effects. Smoking cessation is simply defined as the process of discontinuing tobacco smoking. Current methods of smoking cessation include:
- Unassisted – About 90% of people who try to quit smoking do it without outside support; no aids, therapy or medicine. Although most people try to quit this way, it’s not the most successful method. Only about 4% to 7% can quit on their own. This includes everything from abrupt quitting (‘cold turkey’), gradual reduction to setting the date where they stop smoking.
- Behavioral Therapy – This involves working with a counselor or ex-smokers on finding ways to successfully quit from smoking. The core problem associated with tobacco addiction are often ‘triggers’ (due to stress, cravings, depression, etc.) and finding ways to manage these triggers to reduce dependency on smoking.
- Nicotine Replacement Therapy (“NRT”) – There are many types of NRTs introduced to the market over the years; including nicotine gum, patches, inhalers, sprays, and lozenges. They work by giving you nicotine without the use of tobacco.
- Medications – Bupropion (a type of antidepressant) and varenicline (like ‘Chantix’) are prescription medicines that can help with cravings and withdrawal symptoms.
- Combinations of the above – Smokers are more likely to quit for good if they use a combination of different methods. For example, a smoker can undergo behavioral therapy combined with scheduled NRT.
In most cases, counselling and medication can more than double the chances of successful smoking cessation when compared to unassisted methods.
Current Implications & Challenges
Most low- to middle-income countries lack access to certain medications, either due to costs of transportation, taxes or supply chain issues. And these medications are not always readily available when needed. Putting sheer addiction aside, smoking cessation requires continuous behavioral support from their assigned counselor(s), who cannot always be there 24/7.
In most countries, the combined costs of therapy, counseling sessions and medications drives the majority of smokers to attempt cessation on their own, unassisted.
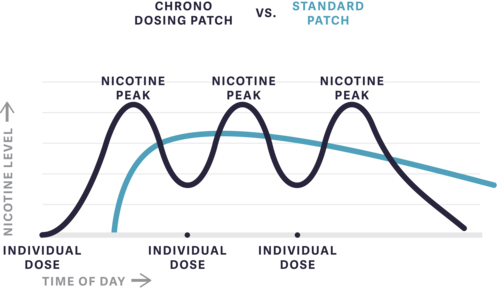
If we take a closer look at the smokers themselves: different smokers have varying profiles (i.e., social smoker, casual smoker, heavy smoker, etc.). Standard NRTs like nicotine patches and gum deliver an inflexible daily dosing profile, regardless of when a smoker may or may not need medication.
There is a need for a solution that effectively addresses the implications mentioned above. A system where patches work intelligently to deliver doses to the smoker at specific times (depending on the profile), while being able to provide continuous behavioral support.
A Smart, Integrated Dosing Solution
A most promising solution to battling tobacco addition is to commercialize a smart, integrated dosing solution. Four key aspects are identified:

- Transdermal Smart Patch – Enhancing on the principles of a nicotine patch, a smart patch would always be attached to the smoker’s arm. Transdermal drug delivery is known to be effective as it eliminates gastro-intestinal absorption or food-drug interactions and has no liver metabolism. It works by delivering accurate doses of nicotine through the skin, based on the smoker’s profile. Additional features would include refillable cartridges, and a ‘help button’ for the smoker to press if he/she has a craving, or simply needs behavioral support.
- Timed Drug Delivery – With a mobile app that gathers data to work together with the smart patch, doses of nicotine can be administered via the patch at specific times of the day. This would offer a more flexible dosing solution catering to various smoker profiles.
- Data Analytics – Every time a dose is administered and every time a craving is recorded, the data is collated to allow the system to provide analytical feedback. This includes content such as days used, circumstances around when the wearable help button is triggered, etc. This would profoundly affect a therapy’s potential.
- Mobile App – Aside from reminding the smoker to refill the smart patch’s drug cartridges, this mobile app would help ensure the smoker to stay on track. An intuitive behavioral support comprises various aspects such as proactive reminders, clinical education, personalized motivators and just-in-time help. Furthermore, sensors embedded into the smart patch would allow for compliance monitoring and assistance.
Enter Chrono Therapeutics
Xeraya Capital is working closely with Chrono Therapeutics in developing a clinically tested smoking cessation program to help people quit for good. This is achieved by having an integrated dosing solution to help smokers battle the addiction to tobacco use. And the program is expected to help smokers quit within as little as 10 weeks. For more information, view and download our SlideShare on smoking cessation.