What Are Vaccines?
A vaccine is a biological substance that’s designed to protect humans from infectious diseases caused by viruses or bacteria (‘pathogens’). It’s different from therapeutic drugs in the sense that it works with our immune system to prevent specific infections.
Vaccines are critical in developing our immunity towards dangerous pathogens, in a sense that it stops the pathogens from infecting and spreading in our body before we can spread it to others. In the long run, vaccines effectively stop the spread of an infectious disease.
Understanding Our Immune System
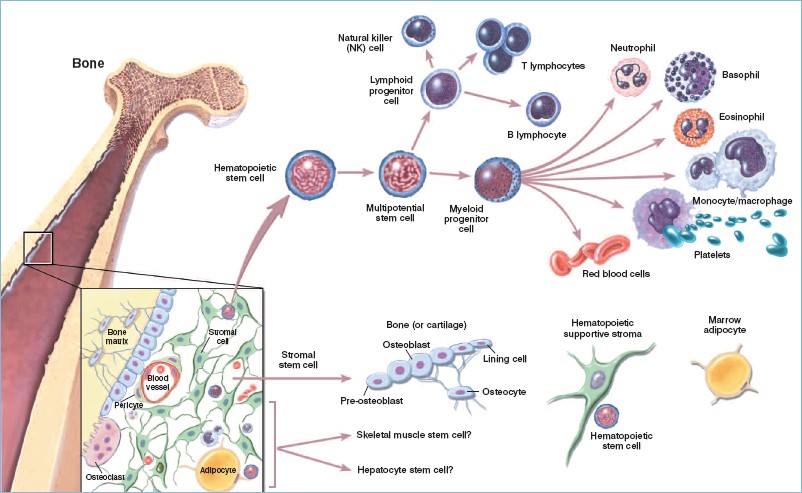
Before we can proceed to understand how vaccines work, we must first consider how our immune system protects us from infections. First and foremost, it is a complex network of cells and proteins that move through our blood and tissue throughout the body.
The main parts of the immune system include white blood cells, antibodies, lymphatic system, spleen, bone marrow and thymus.
Our blood contains red blood cells (that carry oxygen to tissues and organs), and white cells for fighting infections. These white ‘immune’ cells consist primarily of macrophages, B-lymphocytes and T-lymphocytes:
- Macrophages – white blood cells that swallow up and digest pathogens, plus dead or dying cells. They leave behind parts of the digested pathogens called antigens. The body identifies antigens as dangerous and stimulates antibodies to attack them.
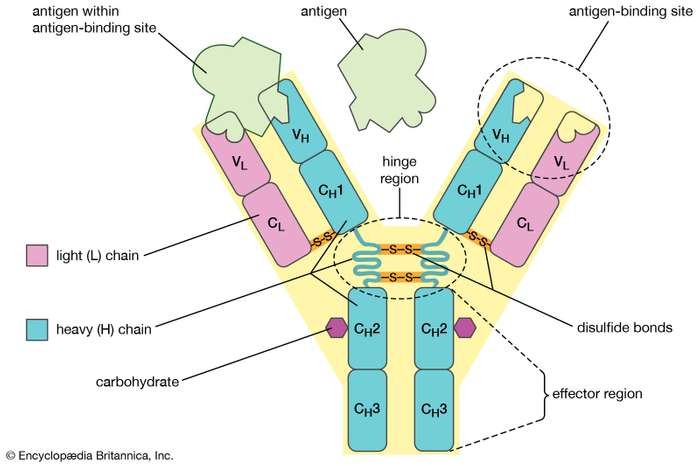
- B-lymphocytes – defensive white blood cells. These small ‘factories’ produce Y-shaped proteins called ‘antibodies’ that bind to and neutralizes antigens left behind by the macrophages.
- T-lymphocytes – another type of defensive white blood cell. They are comprised of 3 types that work together to attack cells in the body that have already been infected.
How White Cells Fight Infection
When a pathogen (either bacteria or virus) invades our body, our immune system is quick to recognize them as invaders. This is because the proteins or sugars on the pathogen’s surface (called ‘antigens’) have different shapes that would bind to any of the cells in the human body, via ‘receptors’.
Upon binding of these receptors to a specific antigen, a complex chain of events is triggered, involving many different types of white blood cells working together.
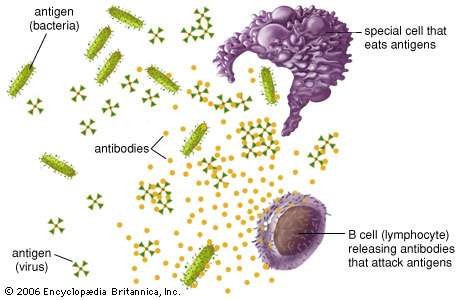
Macrophages engulf, digest and breakdown the pathogens, and then present the antigens on its cell surface. This would signal the presence of antigens to corresponding ‘helper’ T-lymphocyte cells.
The helper T-cells would then stimulate B-lymphocyte cells to multiply and make the corresponding antibodies. These antibodies stick to the pathogen that would either kill (bacteria) or disable them (virus).
Helper T-cells also triggers the cytotoxic ‘killer’ T-cells to attack infected cells. This entire process cascades and repeats itself throughout the infected parts of our body until we eventually recover.
After the infection, our immune system remembers what it learned about how to protect the body against that particular pathogen, and the resulting disease.
The body keeps a few T-lymphocytes, called ‘memory’ T-cells, that would spring into action quickly if the body encounters the same pathogen again. When the familiar antigens are detected, B-lymphocytes produce antibodies to attack them.
Throughout our lifespan, each of us would develop immunity towards various types of diseases. This is essentially an actively acquired natural immunity that we develop after exposure to infection.
Nature Takes Time
During an infection, the ability of our immune system to produce antibodies of the right shape can take several days. Antibodies have to be exactly the right shape – a bit like a key fitting a lock. Our bodies have a library of billions of white blood cells, each of which is limited to making just one shape of antibody.
By this time there could be billions of disease-causing pathogens in our body. It gets worse when a disease is contagious, as it can spread to others who have yet to develop an immunity.
Facilitating Acquired Herd Immunity: Vaccines
Vaccines work with our immune system to safely ‘train’ our bodies to recognize and fight the target pathogens. They contain a weakened or dead form of bacteria or viruses, or even just a few antigens (proteins or sugars) from the surface.
This is sufficient to trigger the immune system that a pathogen has got in. By injecting these antigens into the body, the immune system can safely learn to recognize them as hostile invaders, produce antibodies, and remember them for the future.
Upon administering a vaccine, the same immune process (explained earlier) takes place as when the real pathogens invade our bodies – except this time, you don’t get ill.
Sometimes, after getting a vaccine, the ‘imitation’ infection can cause minor symptoms, such as fever. Such minor symptoms are normal and should be expected as the body builds immunity.
Afterward, if your body ever meets the real thing, your immune system will remember it and get rid of it before you even know it’s there.
Types of Vaccines
The key to vaccines is injecting the antigens into the body without causing the person to get sick at the same time. Scientists have developed several ways of doing this, and each approach makes for a different type of vaccine.
- Live Attenuated – Weaker, non-symptomatic version of a pathogen
- Inactivated – ‘Dead’ pathogens, that would still contain enough antigens to train our immune system
- Subunit/conjugate – An extracted key component of a pathogen (a specific protein or carbohydrate)
- Toxoid – Some bacteria secrete harmful chemicals or toxins when they infect a human body. These chemicals can be ‘deactivated’ and safely be administered as a vaccine
- DNA/RNA – The key component of a pathogen is their genetic material. Modified versions of these strands would instruct the immune system to produce antigens, and consequently combat them all by itself.
- Recombinant Vector – Similar to DNA/RNA vaccines, except that the genetic material uses a modified bacterium or virus as a ‘ride’ (vector).
Measuring The Effectiveness Of A Vaccine
During the development of any type of vaccine, the United States Food & Drug Administration usually takes into account two important factors:
- T-cell response – this indicates the vaccine’s ability to signal T-cells to trigger other white cells to fight the disease, either triggering ‘killer’ T-cells to attack other infected cells or trigger B-cells to produce antibodies.
- Antibody response – this indicates the effectiveness of the modified antigen to trigger B-cells to multiply and produce the corresponding antibodies.
In most cases, most patients require two doses of a vaccine for the effective prevention of an outbreak. Some diseases like certain strains of influenza require vaccines to be administered on an annual basis.
Vaccines Drive Herd Immunity
While vaccines are essentially effective for an individual’s state of health. More importantly, they can protect entire communities. Once enough people are immunized, opportunities for an outbreak of disease become so low even people who aren’t immunized benefit.
In a nutshell, the target pathogen simply won’t have enough people to infect, moreover to spread further, and will eventually die out entirely. This phenomenon is called ‘herd immunity’ or ‘community immunity’. Vaccines have an effective track record of eliminating devastating diseases, without even vaccinating every single person.
This is critical because there will always be a percentage of the population that cannot be vaccinated: infants, young children, the elderly, people with severe allergies, pregnant women, or people with compromised immune systems.
Thanks to herd immunity, these people are kept safe because diseases are never given a chance to spread through a population.
Public health officials and scientists continue to study herd immunity and identify key thresholds. An average vaccination rate of 70% has proven to be successful.
Sources:
- https://vk.ovg.ox.ac.uk/vk/how-do-vaccines-work
- https://www.healio.com/hematology-oncology/learn-immuno-oncology/the-immune-system/components-of-the-immune-system
- https://www.livescience.com/32617-how-do-vaccines-work.html
- https://www.publichealth.org/public-awareness/understanding-vaccines/vaccines-work/
- https://www.britannica.com/science/antibody
- https://www.cdc.gov/vaccines/hcp/conversations/downloads/vacsafe-understand-color-office.pdf
- https://www.healthline.com/health/acquired-immunity
- https://www.healthline.com/health/lymphocytes
- https://www.winchesterhospital.org/health-library/article?id=222982
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/immune-system
- https://www.healthdirect.gov.au/immune-system
- https://www.nationalgeographic.com/science/2020/05/moderna-coronavirus-vaccine-how-it-works-cvd/