A Rare & Progressive Disorder in Need of Breakthrough
Pulmonary arterial hypertension (PAH) is a rare and progressive disorder. It is a specific type of pulmonary hypertension that is caused when the smaller arteries in the lungs become thickened and narrowed. This narrowing blocks the blood flow through the lungs, raising the blood pressure. It eventually forces the heart to work harder and over time the heart loses the ability to effectively pump blood throughout the body, causing heart failure and death.
What Causes Pulmonary Arterial Hypertension?
While the obstruction within the small arteries in the lung can be caused by a variety of reasons, the exact cause of PAH is unknown.
- If the cause of this change is unknown it is referred to as idiopathic PAH.
- If the change is believed to be caused by a genetic mutation it is called heritable PAH. Approximately 15-20% of PAH patients have heritable PAH.
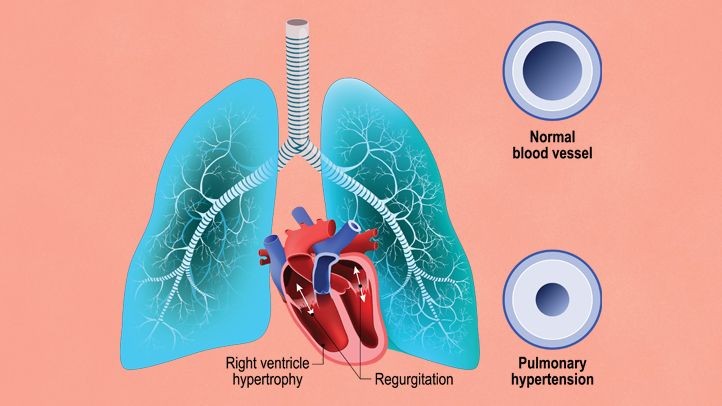
It is unlike other forms of pulmonary hypertension, where high blood pressure in the lungs is caused by underlying heart or lung disease. Researchers believe that PAH occurs when there is an injury to the cells that line the blood vessels of the lung, which over time results in this blood vessel disease. The World Health Organization (WHO) classifies PAH as ‘Group 1 PH’.
What Are the Symptoms of PAH?
In the early stages of PAH, the patient may not notice any symptoms at all, until the disease progresses. Emerging symptoms as it progresses are similar to other lung diseases such as asthma, emphysema or chronic obstructive pulmonary disease (COPD). The most commonly known symptoms of PAH are:
- Increased shortness of breath
- Fatigue
- Edema, or swelling of the feet, legs and eventually the abdomen and neck
- Dizziness and fainting spells
- Chest pain
- Heart palpitations (racing or pounding)
- Lips and fingers turning blue
Notice that most of the symptoms listed above are similar to other common lung diseases, making it challenging to properly diagnose PAH. Both lung and heart specialists (pulmonologist and cardiologist) will need to conduct several tests on the patient. These include testing the patient’s blood, electrocardiogram, breathing, 6-minute walk, echocardiogram (ultrasound of the heart) as well as right-side heart catheterization (insertion of a catheter or small tube into the body to measure blood pressure in the lungs).
What Are the Risk Factors & Prevalence?
Known conditions that are associated with the development of PAH include:
- Connective tissue disorders – scleroderma and lupus
- Exposure to certain toxins and drugs – like methamphetamine and cocaine
- Infections – including HIV and schistosomiasis (a disease caused by parasitic worms)
- Cirrhosis of the liver
- Congenital heart abnormalities (due to birth defects that affects how the heart works)
PAH occurs more frequently in women than in men by about 3-5 times. Somehow, women between the ages of 30 and 60 are more susceptible. New cases are estimated to occur in one to two individuals per million each year in the U.S and are estimated to be similar in Europe. Approximately 500 to 1,000 new cases of PAH are diagnosed each year in the U.S.
Prevalence commonly ranges from 15 to 25 per million people within the U.S and Europe. There is no ethnic or racial group that is known to have a higher frequency of patients with PAH.
According to Lancet in 2016, pulmonary hypertension affects up to 70 million people worldwide.
How do We Treat Patients with PAH?
Until now, there is no specific cure for PAH. There are, however, medications and procedures to slow the progression of the disease and improve the patient’s chances of coping with normal everyday life. PAH-specific medications include:
- Oral treatments that prevent blood vessels from narrowing, allowing the lungs to relax
- Intravenous treatments that open up the blood vessels to help ease the chest pain and shortness of breath
- Subcutaneous treatments that use portable infusion pumps to open up the blood vessels
- Inhaled treatments to relieve shortness of breath
- Pulmonary rehabilitation – exercises to rebuild strength and improve lung function
- Other supportive treatments such as diuretics (medications that increase water and salt expelled via urine), anticoagulants to prevent blood clots and having a portable oxygen tank ready
- In some severe cases, a lung transplant may be recommended
Aside from the above treatments and medications, PAH patients should also make adjustments to their lifestyle, such as not smoking, staying active with light exercises, avoid high-altitude activities (including hiking) and eating healthy. For women, they may need to discuss the matter of pregnancy with the doctor as it puts a strain on the body.
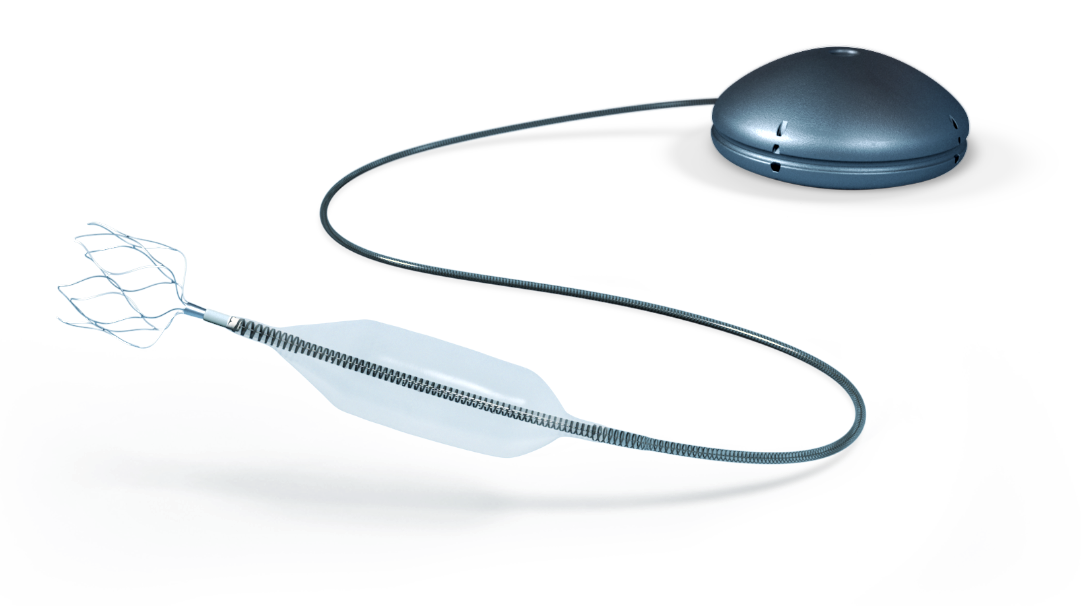
Aria CV’s PH System: A Novel Implantable Device
Aria CV (founded in 2010) has come up with a novel device that can be implanted as such that it can mimic the function of healthy vessels. The device works by inserting a gas-filled balloon into the main pulmonary artery that is connected by a catheter to a hollow reservoir. This restores compliance to the pulmonary vessels, enabling the heart to pump more blood for less energy.
Therefore, the patient’s ability to perform daily activities (including exercises) is improved, and yet the burden on the heart is reduced. The implant procedure is similar to existing cardiac devices that are already established.
Aria CV has already performed its first clinical study in Vienna, and the U.S Food and Drug Administration (FDA) has granted Breakthrough Device Designation for their Pulmonary Hypertension System.
Liquidia’s LIQ861 Treprostinil Inhalation Powder
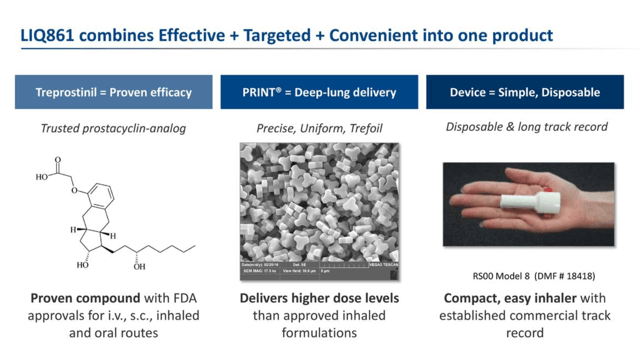
Liquidia is a biopharmaceutical company focused on the development and commercialization of products that are directed towards the treatment of pulmonary arterial hypertension (PAH). Their most promising candidate, LIQ861 (an inhaled dry powder formulation of treprostinil) is undergoing Phase 3 trials with the FDA.
Treprostinil is a vasodilation type drug that widens the blood vessels. Liquidia’s proprietary PRINT® Technology enables the manufacturing of highly uniform particles of the drug that enhances the drug delivery deep into the patient’s lungs. This allows for a more potent (and effective) dose compared to currently available inhaled therapies.
Summary
Pulmonary arterial hypertension (PAH) is a rare, progressive disorder (meaning it gets worse over time), in which the cause is usually unknown. It is most common in women between the ages of 30-60. There is no specific cure for PAH, but treatments are available to control symptoms and improve quality of life. Aria CV is developing a novel implantable device that would allow the heart to pump more blood for less energy, it has received Breakthrough Device Designation from the FDA. Liquidia’s inhaled dry powder formulation of treprostinil (LIQ861) helps to widen the blood vessels and is currently in Phase 3 of clinical trials.
Sources:
- https://www.everydayhealth.com/pulmonary-arterial-hypertension/
- https://www.lung.org/lung-health-diseases/lung-disease-lookup/pulmonary-arterial-hypertension
- https://rarediseases.org/rare-diseases/pulmonary-arterial-hypertension/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7000864/
- https://www.nhs.uk/conditions/pulmonary-hypertension/treatment/
- https://ariacv.com/technology/
- https://www.liquidia.com/products-and-pipeline/overview