An Overview of Key Figures, Implications, and the Need for New Antibiotics
We’ve mentioned before how antibiotics are critical in saving millions of lives every day through the treatment of bacterial infections. It is also vital in preventing infections, especially for patients who are about to undergo medical surgery, chemotherapy, or labor.
In this article, we’ll be discussing how bacterial antimicrobial resistance (AMR) is becoming a clear and present threat to global healthcare, and how we should all work together to combat AMR.
By The Numbers
A recent study co-funded by Bill & Melinda Gates Foundation (published by The Lancet in January 2022) estimated that 4.95 million deaths were associated with bacterial AMR in 2019. 1.27 million of which were a direct result of antibiotic-resistant bacterial infections in the 88 pathogen–drug combinations evaluated.
To put things in perspective, The Review on Antimicrobial Resistance (published in 2016) previously estimated that as many as 10 million people could die annually from AMR by 2050.
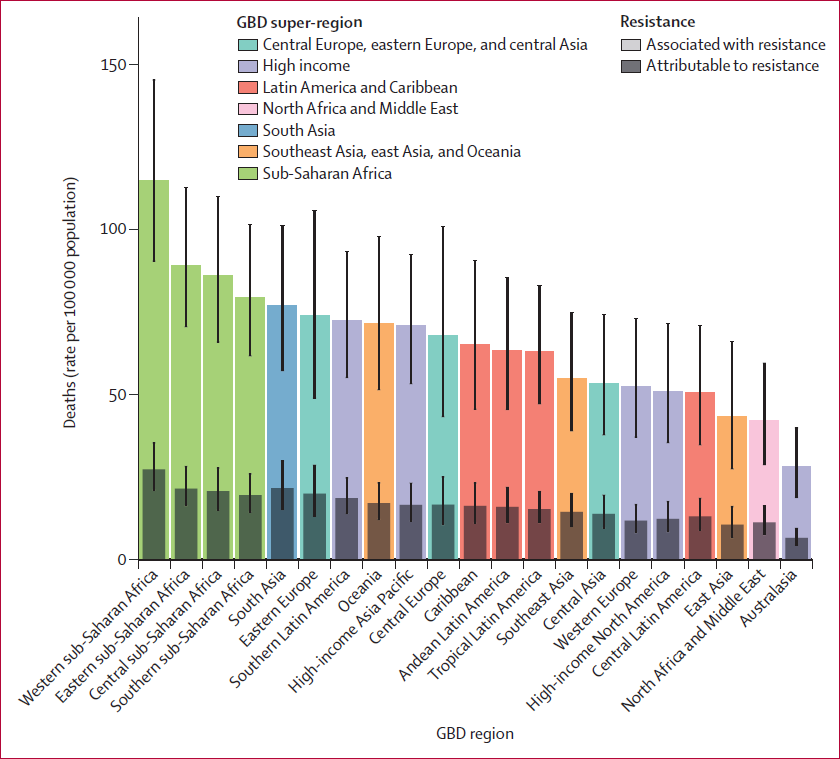
All-age rate of deaths attributable to and associated with bacterial AMR in 2019 (The Lancet, Jan 2022)
Bacterial AMR is a problem in all regions; in 2019, the highest rates of AMR burden were in sub-Saharan Africa, with 27.3 deaths per 100,000 attributable to AMR and 114.8 deaths per 100,000 associated with AMR. Australasia had the lowest AMR burden in 2019, with 6.5 deaths per 100,000 attributable to AMR and 28.0 deaths per 100,000 associated with AMR.
On another note, 200,000 newborns die each year from drug-resistant infections.
Narrowing Down The Pathogens
Three infectious diseases dominated the global burdens attributable (direct cause) to and associated (indirect) with AMR in 2019:
- lower respiratory and thorax infections
- bloodstream infections
- intra-abdominal infections
When combined, these diseases accounted for 78.8% of deaths attributable to AMR in 2019; lower respiratory infections alone accounted for more than 400,000 attributable deaths and 1.5 million associated deaths.
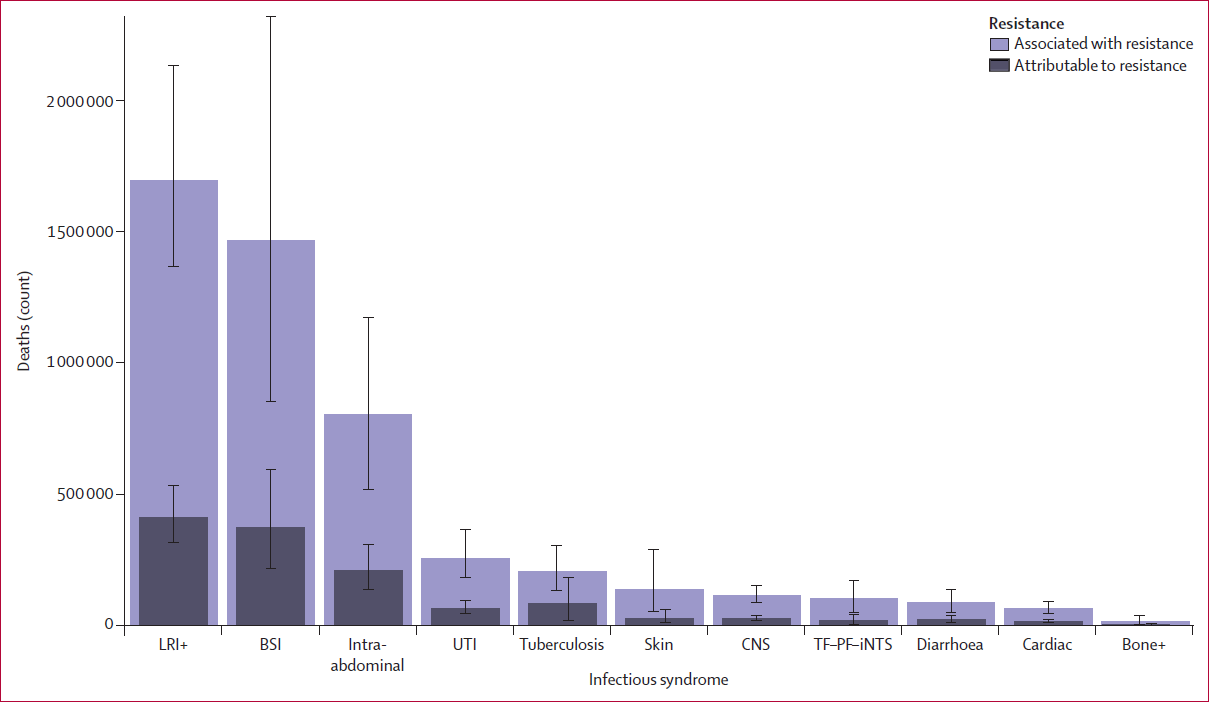
Global deaths attributable to and associated with bacterial AMR by infectious disease in 2019 (The Lancet, Jan 2022)
Zooming in, six pathogens were each responsible for more than 250,000 deaths associated with AMR (by order of the number of deaths caused): E coli, Staphylococcus aureus, K pneumoniae, S pneumoniae, Acinetobacter baumannii, and Pseudomonas aeruginosa.
Together, these six pathogens were responsible for 929,000 of 1.27 million deaths attributable to AMR and 3.57 million of 4.95 million deaths associated with AMR globally in 2019.
Seven pathogen-drug combinations each caused more than 50,000 deaths.
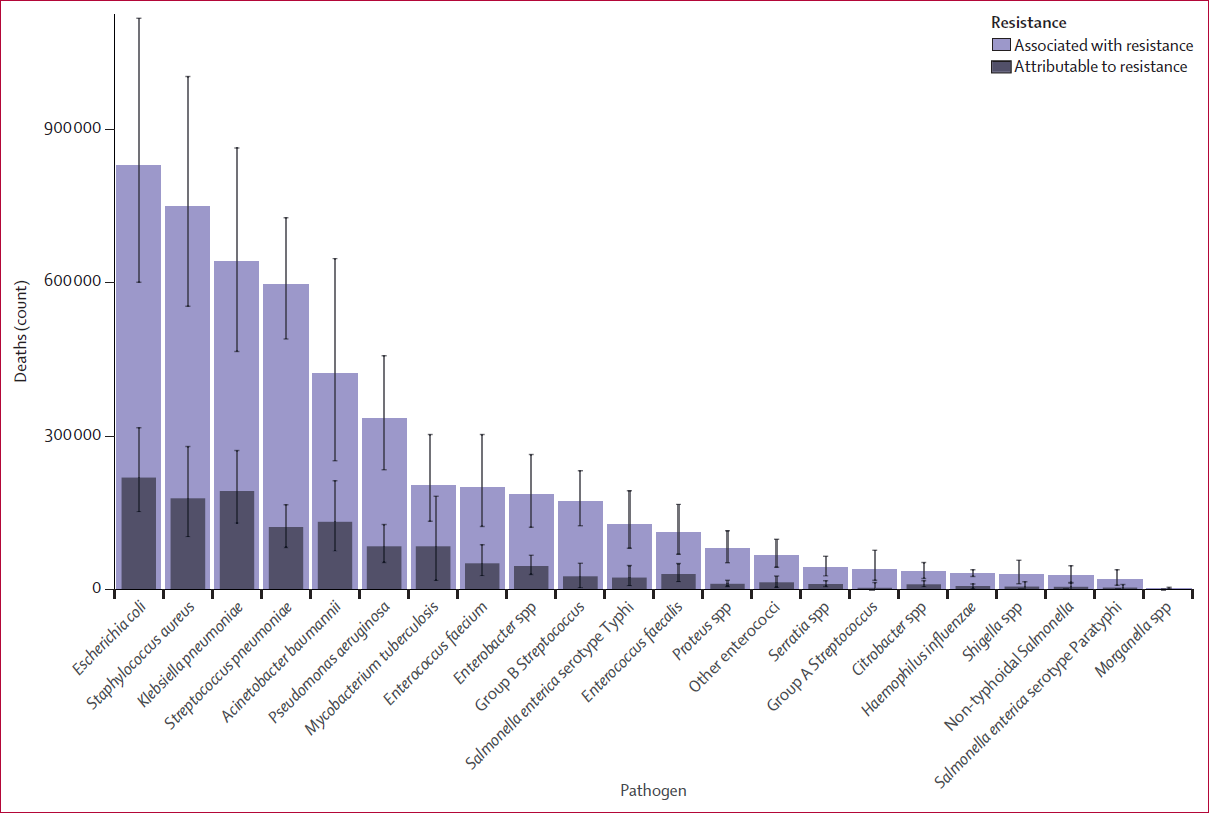
Global deaths attributable to and associated with bacterial AMR by pathogen in 2019 (The Lancet, 2022)
The Long Term Implications of AMR
The United Nations established 17 interlinked global Sustainable Development Goals (SDG) in 2015. These SDGs were designed to be a “blueprint to achieve a better and more sustainable future for all”.
Policymakers would soon realize that AMR is a central issue to several SDGs. For example, for SDG 1 (no poverty), AMR could cause an additional 28.3 million people to be pushed into extreme poverty by 2050 due to high costs of treatment and chronic infections. As a case example, in the United States alone, antibiotic resistance could add about USD 1,400 to the hospital bill for treating patients with any bacterial infections (according to the CDC).
On SDG 2 (zero hunger), animals harmed by AMR affect farmers’ livelihood and broader food security. On SDG 8 (decent work and economic growth), as AMR increases mortality and morbidity, labor supply will decline and could cause a decrease of 1-3% in global economic output by 2030, amounting to losses of up to USD 3.4 trillion.

An infectious disease ward (WHO, 2020)
The Need for a Global Assessment Authority on AMR
In 2017, WHO published a priority list for developing new and effective antibiotic treatments. The list was intended to inform research and development priorities related to new antibiotics and put the most emphasis on pathogens with multidrug resistance that cause severe and often deadly infections in healthcare and nursing home settings.
Only five of the seven pathogen-drug combinations that caused the most deaths attributable to bacterial AMR in 2019 are currently on the list; MDR tuberculosis and fluoroquinolone-resistant E coli are not included. In fact, the first SDG indicator for AMR was only proposed in 2019, and this indicator (3.d.2) is very limited in scope.
Estimates of the burden of bacterial AMR to date, clearly show that drug resistance in each of the leading pathogens is a major global health threat that warrants more attention, funding, capacity building, research and development, and pathogen-specific priority setting from the broader global health community. Thus, there is a need for a global assessment authority specifically meant for bacterial AMR.
Here’s something else to think about, antibiotic development is imperative to outpace the ability of bacteria to develop resistance. As of July 2021, only 17 new systemic antibiotics and one related biologic have been approved by the FDA since 2010. Among these drugs, 14 were approved for common bacterial infections.
Recommended Intervention Strategies
Intervention strategies for addressing the challenge of bacterial AMR fall into five main categories:
- Prevention & control of infection – this would be the foundation for preventing infections broadly and a cornerstone in combating the spread of AMR. It ranges from basic aspects such as water, sanitation, and hygiene to preventing and controlling hospital-acquired infections.
- Vaccination – preventing infections through vaccinations is paramount for reducing the need for antibiotics. Vaccines are available for only one of the six leading pathogens (S pneumoniae), although new vaccine programs are underway for S aureus, E coli, and others. Therefore, vaccine development is crucial for pathogens that currently have no vaccine.
- Reducing exposure to antibiotics – especially those unrelated to treating human disease is an important potential way to reduce risk. Increased use of antibiotics in farming has been identified as a potential contributor to AMR in humans, although the direct causal link remains controversial.
- Minimizing the use of antibiotics – particularly when they are not necessary to improve human health (such as treating viral infections) should be prioritized. To this end, building infrastructure that allows clinicians to diagnose infection accurately and rapidly is crucial so that antimicrobial use can be narrowed or stopped when appropriate.
- Maintaining investment in the development of new antibiotics – as well as access to second-line antibiotics in locations without widespread access is essential. In recent decades, investments have been small compared with those in other public health issues with similar or less impact. Given the global importance of bacterial AMR, more assessment of which policies have worked, and where, is urgently needed.
Summary
The topic of AMR should not be taken lightly, recent studies found that bacterial AMR is a global health problem whose magnitude is at least as large as major diseases including HIV and malaria, and potentially much larger in coming years.
Sources
- https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)02724-0/fulltext
- https://journals.sagepub.com/doi/10.1177/10600280211031390
- https://www.who.int/publications/i/item/9789240021303
- https://www.theguardian.com/society/2022/jan/20/antimicrobial-resistance-antibiotic-resistant-bacterial-infections-deaths-lancet-study
- https://sdgs.un.org/goals
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6929930/
- https://www.nhs.uk/conditions/antibiotics/uses/